Written by Brandon Okey. Mina Draskovic, B.Psy., reviewed this content for accuracy.
The liver is one of the body’s most vital organs, and it just so happens to suffer the most from heavy drinking. Excessive alcohol consumption can cause fat deposit build-up, inflammation, scarring, and liver cell death—all of which are significant risk factors for liver disease and cancer.
The sooner you quit drinking, the better for your liver and the rest of your body.
If you find yourself unable to control your drinking habits, we can help. Our alcohol rehab teaches you how to rewire your patterns, body, and brain for an addiction-free life, while our alcohol detox program ensures a safe recovery journey.
If you’re struggling, don’t hesitate—recovery is within reach.
Ardu has highly exceptional staff that truly love their jobs and care about the clients treating them with the utmost love and respect. After graduating from Ardu in October, I am proud to report that I am still clean and sober six months later. The tools I learned at Ardu are tools I can take with me for a lifetime.
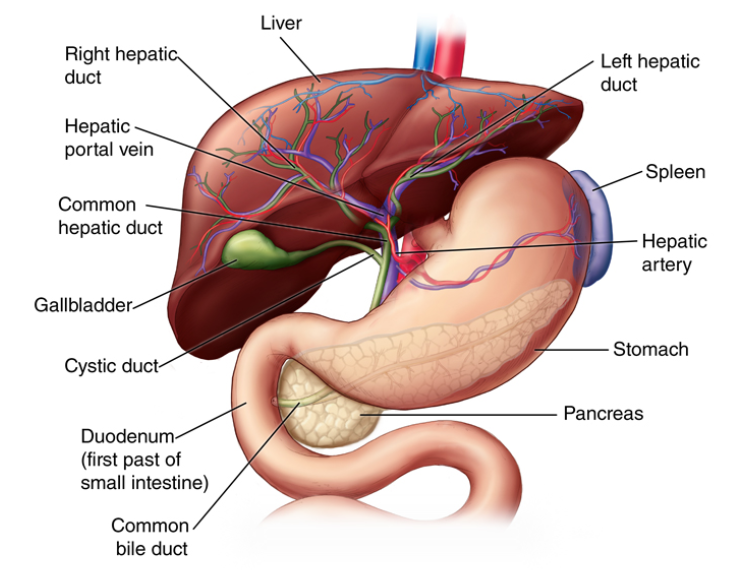
The liver is an organ located on the right side of the body just below the ribs. It performs hundreds of essential functions vital for sustaining life. On average, the liver weighs about three pounds, making it the largest internal organ.
A healthy liver is important for:
Unlike other organs, your liver can regenerate. The National Institutes of Health reveals that the liver can grow new cells to repopulate damaged areas and completely restore lost function, even if up to 90% of the liver is removed or damaged.
One of the greatest foes to your liver is alcohol. Excessive alcohol consumption is a leading cause of liver disease, preventing it from effectively regenerating and causing severe damage.
The best way to help your liver recover and thrive is to abstain from alcohol consumption. Contact Ardu today to start your recovery.
Excessive drinking can have a variety of adverse effects on your liver in a short time. Signs of liver damage may be quick to appear after periods of chronic alcohol abuse.
Early symptoms of alcoholic liver damage include:
If you have a history of excessive drinking, don’t wait for the physical symptoms of addiction to go too far. Read more about the tell-tale signs of alcoholism to learn what to watch for.
Alcohol begins affecting liver function almost immediately after consumption. Some negative effects start showing as soon as ethanol (the intoxicating substance in alcoholic drinks) reaches the liver to be processed. It’s no wonder you often feel the consequences of one wild, booze-filled night even a few days after.
Here are some of the major short-term effects of alcohol on the liver:
If this is the toll alcohol takes on your liver after just one night of heavy partying, imagine the extent of alcohol’s detrimental effects on your liver in the long run.
If you are a habitual heavy drinker, the negative effects of alcohol will eventually cause more severe and permanent liver damage. The persistent presence of alcohol toxicity and inflammation prevents cell regeneration between episodes of overindulging. Bit by bit, damage accumulates past the liver’s ability to fully recover, eventually leading to liver failure.
Here’s what happens to your liver after chronic heavy drinking.
Heavy alcohol consumption may produce leakage of microbes and microbial products from the gastrointestinal tract, which quickly reach the liver via the portal vein. Exposure to these immune challenges and to alcohol and its breakdown products dysregulates the liver’s normally fine-tuned immune signaling pathways. (Nagy, Ph. D.)
There’s no way around it: the best thing you can do for yourself is to lay off the booze.
The first few weeks after quitting may be the hardest, as alcohol withdrawal symptoms set in. Your liver tries to recover—and the rest of your body too. We’re here to facilitate your recovery and hold your hand every step of the way at our drug and alcohol rehab center.
Alcohol metabolism places substantial stress on the cells, which can inflict progressively severe damage in chronic heavy drinkers. Let’s not forget that the process of breaking down alcohol also generates toxic byproducts that further damage liver cells. People who regularly consume excessive amounts of alcohol will eventually develop some form of liver disease.
One of the earliest effects that alcohol has on the liver is the accumulation of fat deposits in liver cells, known as fatty liver disease. As the liver metabolizes alcohol, the chemical byproducts generated interfere with the liver’s ability to break down fats. This causes excess fat to build up inside liver cells.
Continued alcohol consumption use will lead to increased inflammation that will inevitably cause permanent damage.
The liver sustains the greatest degree of tissue injury by heavy drinking because it is the primary site of ethanol metabolism. Chronic and excessive alcohol consumption produces a wide spectrum of hepatic lesions, the most characteristic of which are steatosis, hepatitis, and fibrosis/cirrhosis. (Osna, et. al.)
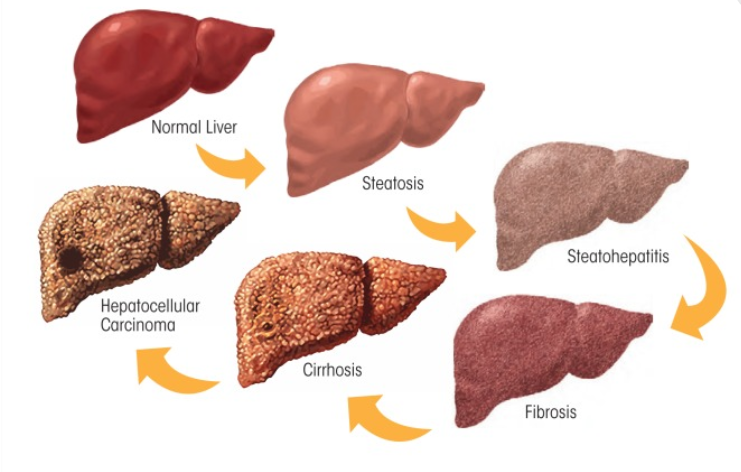
Persistent excessive drinking leads to chronic inflammation in the liver, which is known as alcoholic hepatitis. This recurring inflammation is triggered by repeated exposure to alcohol’s toxic effects and byproducts as the liver metabolizes alcohol.
Osna, et. al. suggest that chronic inflammation also activates molecules such as macrophages, which trigger cell death pathways in liver cells. The ongoing attack results in liver cell death over time and leads to liver fibrosis. Fibrosis impairs blood flow and the replacement of damaged liver tissues.
Alcoholic hepatitis has serious consequences, as the liver’s function is severely compromised. If left untreated, alcoholic hepatitis can progress to liver fibrosis, cirrhosis, and end-stage liver failure.
Inflammation caused by alcohol metabolism can eventually lead to fibrosis or scarring of the liver. Fibrosis occurs because chronic inflammation kills off liver cells, and specialized cells called hepatic stellate cells rush in to repair the damage by laying down collagen and other fibers.
Activated hepatic stellate cells, portal fibroblasts, and myofibroblasts of bone marrow origin have been identified as major collagen-producing cells in the injured liver. These cells are activated by fibrogenic cytokines such as TGF-β1, angiotensin II, and leptin. (Bataller and Brenner)
Over time, this process results in the replacement of healthy liver tissue with non-functioning scar tissue. As fibrosis spreads, toxins, hormones, medications, and waste products cannot be properly metabolized and detoxified. Liver function declines further as scar tissue replaces more functional tissue.
As fibrosis continues to spread through the liver, it eventually leads to the end-stage disease known as cirrhosis. Alcohol-related cirrhosis occurs when most of the liver cells have been replaced with non-functional scar tissue. According to liver research, “up to 50% of cirrhosis-associated deaths are due to alcohol abuse in the US.”
In cirrhosis, the normal soft liver tissue is distorted by fibrotic bands and nodules of hard scar tissue. The circulating blood flow through the liver becomes severely impaired as the remaining liver cells cannot get enough oxygen and nutrients. This can lead to liver failure.
Despite the liver’s ability to regenerate, this extensive cirrhosis scarring cannot be reversed. This is why alcoholic cirrhosis represents a serious threat to life.
It’s painful to witness the struggle that people with alcohol use disorder (AUD) endure. Alcoholic liver disease is the dire end result of unmanaged addiction, but help is within reach. Ardu Recovery Center provides a safe, caring space conducive to rediscovering well-being as you break the patterns of addiction.
Contact us today and discuss your options with one of our caring specialists.
Heavy alcohol consumption has been linked to an increased risk of developing several types of liver cancer. Researchers from Italy have shown that chronic alcohol intake is the most common cause of hepatocellular carcinoma (HCC), responsible for about one-third to nearly half of cases.
…a significant relationship between alcohol intake, metabolic changes, and hepatitis virus infection does exist. Alcohol may be a factor in the development of HCC via direct (genotoxic) and indirect mechanisms (cirrhosis).
The research concluded that if a person stops drinking alcohol, their risk of liver cancer starts to decrease, but it takes a long time, about 23 years, to go back to a lower level.
Here’s how these alcohol-related effects increase the risk of liver cancer:
An ounce of prevention is worth a pound of cure. Abstinence from alcohol is truly the best medicine to halt further DNA damage and inflammation that cause malignancies. Our addiction treatment programs provide the comprehensive medical and psychological support needed to safely manage withdrawal symptoms and build lifelong sobriety habits.
The amount of alcohol that ultimately causes alcoholic liver injury varies from person to person and depends on factors such as:

A 2002 study revealed that “women are at a higher risk of developing liver injury than men, even when factors such as body weight and amount of alcohol consumed are taken into consideration.”
The average threshold alcohol intake to produce liver injury is 40 g/day to 60 g /day (3 to 5 drinks) in men but only 20 g/day (<2 drinks) in women with a drink defined as 12 oz (354 mL) of beer, 5 oz (148 mL) of wine or 1.5 oz (44 mL) of 80-proof distilled spirits, each containing about 12g of alcohol (7,8).
These average thresholds vary among different populations. Bruha, et. al. found that “in the Chinese population, the ethanol risk threshold for developing alcoholic liver disease (ALD) is 20 g per day with the risk increasing in proportion to the daily intake.”
The number of years of drinking it takes to damage the liver also varies from one individual to another, and depends on the list of factors previously mentioned. Research suggests that heavy drinking for more than ten years is generally associated with a much higher risk of liver disease.
Mayo Clinic suggests that “of heavy drinkers, 10%–20% develop cirrhosis, a serious condition that usually develops after 10 or more years of drinking.”
…cirrhosis does not develop below a lifetime alcohol consumption of 100 kg of undiluted alcohol. This amount corresponds to an average daily intake of 30 grams of undiluted alcohol for 10 years. Heavy alcoholics consuming at least 80 g of alcohol per day for more than 10 years will develop liver disease at a rate of nearly 100%. (Bruha, et. al.)
Liver damage can occur even with shorter periods of heavy or binge drinking. The best way to prevent liver damage is to consume alcohol in moderation or abstain entirely.
Because of its remarkable regenerative abilities, your liver can heal when you stop drinking. Thomes, et. al. suggest that “even after years of heavy alcohol use, the liver has a remarkable regenerative capacity and, following alcohol removal, can recover a significant portion of its original mass and function.”
Here’s what happens when you finally ditch the bottle:
Give it enough time and see how your liver rebuilds itself from the inside out when alcohol is no longer impairing regeneration.
Here are some signs that your liver may be on the path to recovery:
If you or someone you know is struggling with alcohol-related issues, seek help. Early intervention and treatment can be effective in managing alcohol abuse or addiction. You don’t have to face them alone.
If you’re ready to take the first step toward a healthier, alcohol-free life, reach out today.
Navigating an alcohol addiction can be extremely difficult. The stages of alcoholism ramp up gradually, so it’s difficult to accurately assess your level of addiction. If you’d like to reap the numerous health benefits of sobriety but are unsure of how to stop drinking, your first step is to contact the experts at Ardu.
Our skilled medical professionals are dedicated to providing you with the personalized care you need to successfully navigate this challenging time. We offer:
We tailor our rehab programs to each individual’s needs so that you can achieve success no matter what challenges you may face. Come visit us in Provo, Utah, and let’s discuss how to make your recovery journey as safe, comfortable, and effective as possible.

Brandon Okey is the co-founder of Ardu Recovery Center and is dedicated to empowering people on their journey to sobriety.
If alcohol consumption continues despite established cirrhosis, the liver will experience progressive destruction leading eventually to complete liver failure. The areas of fibrosis will expand, impeding blood flow and essential metabolic functions, causing complications like hemorrhaging blood vessels, fluid retention, and toxins affecting the brain. Mortality risk becomes very high without a liver transplant.
A transplant is challenging with ongoing drinking. Essentially once significant cirrhosis develops, the persistence of drinking will further ravage and shut down liver performance until fatal.
The earliest signs of alcoholic liver damage tend to be subtle or nonspecific such as:
As liver injury progresses, more evident signs arise:
Even advanced liver disease can develop without overt symptoms until sudden complications like variceal bleeding or hepatic encephalopathy arise. It’s important to get regular physicals and blood tests to detect emerging issues.
If you continue to consume alcohol despite alcoholic fatty liver disease, you’re allowing ongoing inflammation, cell death, and scar tissue generation. This results in the progression of alcoholic hepatitis with swelling, substantial cell necrosis, jaundice, and fever.
Persisting habits exacerbate this liver cell damage, eventually causing extensive fibrosis and micronodular cirrhosis. The recurrent injury also increases the risk of liver cancer. Ultimately, the destruction of functional liver tissues evolves into advanced cirrhosis and total liver failure if drinking with a fatty liver condition persists.
The liver possesses remarkable regenerative powers capable of restoring lost function even after significant injury if alcohol use is halted. Healing potential is highest for those who quit drinking in the steatosis or mild alcoholic hepatitis phases before collagenous scarring develops.
Fibrosis and stable cirrhosis also show some potential to regress and stabilize if drinking fully ceases. In all phases, lasting abstinence supports healthy hepatocyte regrowth, reversal of inflammation, improvements in liver enzymes, and synthetic functionality. Reversal capacity does decrease in the end stages or with cirrhosis complications.
The best indicators of satisfactory liver status are the absence of overt clinical symptoms combined with normal results on standard blood tests assessing liver enzymes, proteins, bilirubin, and nutritional biomarkers. Additionally, liver imaging modalities detecting fibrosis and clinical scoring systems such as APRI and Fibrosis-4 can evaluate for advanced liver disease if alcohol use history warrants deeper assessment. Normal scores indicate preserved liver function despite past higher-risk behaviors.
The 4 classic warning signs of a damaged liver are jaundice (yellow skin and eyes), ascites (fluid accumulation in the abdomen), easy bleeding and coagulation impairment, and hepatic encephalopathy (a spectrum of neuropsychiatric disturbances from toxins reaching the brain). The presence of any of these “red flags” indicates advanced liver dysfunction requiring urgent evaluation and treatment.
The rate of alcohol ingestion significantly influences the liver’s response. Drinking alcohol at a slower pace over several hours enables the liver to metabolize ethanol into acetaldehyde intermediates and then to acetate at a manageable rate. This prevents sudden spikes in reactive metabolites that drive acute toxicity when higher volumes are processed rapidly during binge drinking. Moderating intake volume combined with breaks in between drinks gives the liver more of a chance to detoxify without becoming overwhelmed.
While staying well-hydrated supports overall health and liver function, water itself does not “cleanse” the liver or directly remove alcohol metabolites and cellular debris after drinking. The liver cells handle detoxification and waste disposal duties through enzymatic chemical conversions, packaging toxins for kidney elimination, and immune cell digestive processes for the removal of dead cells. Water intake enables these processes but does not actively reduce damage. Only liver cells can truly repair and regenerate liver tissues.
Stage 1 of alcoholic liver disease refers to steatosis or “fatty liver”, which is characterized by lipid droplet accumulation inside liver cells. It is also often referred to as alcoholic fatty liver disease. Liver enzymes are often normal to mildly elevated. Fatty liver typically resolves if a person achieves sobriety before it can progress to more concerning inflammatory states causing cell death and collagen proliferation. Catching ALD early and stopping alcohol intake allows for significant liver regeneration.
Signs that liver health may be deteriorating or damaged include fatigue, nausea, poor appetite, weight loss, jaundice (yellow skin/eyes), enlarging or distending abdomen, prominent spider veins, and unusual bruising or bleeding. It is also characterized by changes in mental activity like sleepiness or confusion, and abnormal blood tests showing elevated bilirubin, liver enzymes (ALT/AST), or prolonged INR/PT. The presence of such clinical indicators warrants medical evaluation for possible liver dysfunction.
Cells that maintain and repair the liver identified. (2021, March 16). National Institutes of Health (NIH). https://www.nih.gov/news-events/nih-research-matters/cells-maintain-repair-liver-identified
Maher, J. J. (1997). Exploring Alcohol’s Effects on Liver Function. Alcohol Health and Research World, 21(1), 5-12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6826796/
Vogt, B. L. (2007). Glutathione Depletion and Recovery After Acute Ethanol Administration in the Aging Mouse. Biochemical Pharmacology, 73(10), 1613. https://doi.org/10.1016/j.bcp.2007.01.033
Barve, S. (2017). Development, Prevention, and Treatment of Alcohol-Induced Organ Injury: The Role of Nutrition. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5513692/
Derdak, Z., & Wands, J. R. (2012). Alcohol, insulin resistance and the liver–brain axis. Journal of Gastroenterology and Hepatology, 27(0 2), 33. https://doi.org/10.1111/j.1440-1746.2011.07023.x
Nagy, L. E. (2015). The Role of Innate Immunity in Alcoholic Liver Disease. Alcohol Research: Current Reviews, 37(2), 237-250. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4590620/
Osna, N. A., & Kharbanda, K. K. (2017). Alcoholic Liver Disease: Pathogenesis and Current Management. Alcohol Research: Current Reviews, 38(2), 147-161. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5513682/
Bataller, R., & Brenner, D. A. (2005, February 1). Liver fibrosis. Journal of Clinical Investigation. https://doi.org/10.1172/jci24282
Ohashi, K., Pimienta, M., & Seki, E. (2018, December 1). Alcoholic liver disease: A current molecular and clinical perspective. Liver Research. https://doi.org/10.1016/j.livres.2018.11.002
Testino, G., Leone, S., & Borro, P. (2014, January 1). Alcohol and hepatocellular carcinoma: A review and a point of view. World Journal of Gastroenterology. https://doi.org/10.3748/wjg.v20.i43.15943
Prakash, O., & Nelson, S. (2001). Alcohol and Liver Disease. The Ochsner Journal, 4(4), 241-244. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3400518/
Bruha, R., Dvorak, K., & Petrtyl, J. (2012). Alcoholic liver disease. World Journal of Hepatology, 4(3), 81-90. https://doi.org/10.4254/wjh.v4.i3.81
MBBS, O. M. (2021, September 3). What effect does alcohol have on your health — and your liver? Mayo Clinic Health System. https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/effects-of-alcohol-on-your-health-and-liver
Thomes, P., Rasineni, K., Saraswathi, V., Kharbanda, K. K., Clemens, D. L., Sweeney, S., Kubik, J. L., Donohue, T. M., & Casey, C. A. (2021, January 1). Natural Recovery by the Liver and Other Organs After Chronic Alcohol Use. Alcohol Research. https://doi.org/10.35946/arcr.v41.1.05
What are the effects of alcohol on kidneys?
Can you reverse the harmful effects of alcohol?
What are the long-term effects of alcohol on the brain?
How long does it take to detox from alcohol?
Is there such a thing as an alcoholic personality?
6 steps to overcome your alcohol addiction