Written by Brandon Okey. Mina Draskovic, B.Psy., reviewed this content for accuracy.
When you crack open a cold one, cancer risks are the last thing on your mind. But extensive research shows that even moderate alcohol consumption is linked to an increased likelihood of several types of cancer.
If you’re struggling with alcohol addiction, now might be the perfect time to break the cycle and reduce your chances of getting cancer.
Our alcohol rehab center can help you start your journey toward sobriety in a supportive and compassionate environment.
Ardu was the very best place for me to get the help I needed… They helped me work through my emotions and past trauma…I’m sober and I’m doing pretty good. I did go to a treatment center before Ardu and on day 16, I left against medical advice because I was not helped at all. I’m grateful for everyone at Ardu, I owe them my life. I would refer anyone I know to Ardu.
The evidence is clear: alcohol consumption can significantly increase the risk of cancer. While many are unaware of the connection, the relationship between alcohol consumption and the increased likelihood of cancers is significant enough to prompt major health authorities to officially classify alcohol as a Group 1 carcinogen. That means that alcohol is one grouped with the most dangerous cancer-causing agents.
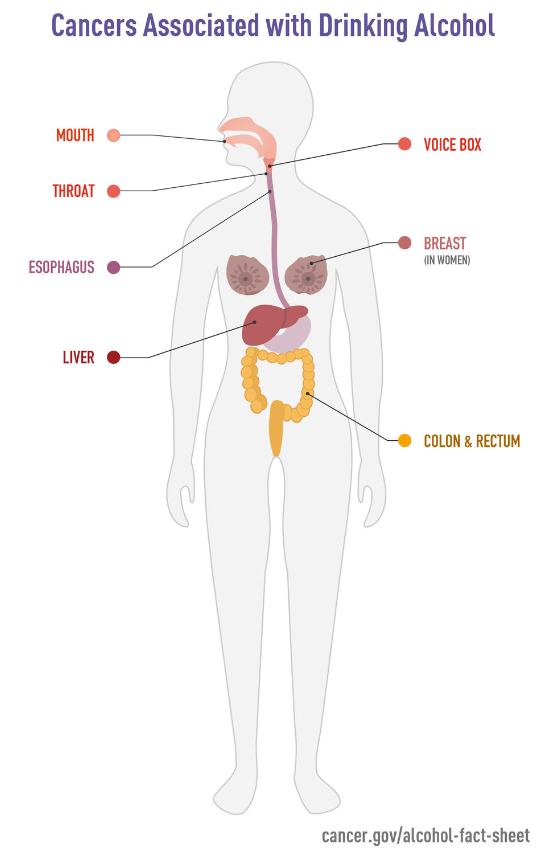
A 2020 global study found that about 4.1% of all new cancer cases worldwide were caused by alcohol consumption. Cancers of the esophagus, liver, and breast were the most commonly linked to alcohol. The study also showed that the more alcohol a person drinks, the higher their risk of alcohol-related cancers.
The World Health Organization warns that “no level of alcohol consumption is safe for our health.”
Alcohol is a toxic, psychoactive, and dependence-producing substance and has been classified as a Group 1 carcinogen by the International Agency for Research on Cancer decades ago – this is the highest risk group, which also includes asbestos, radiation and tobacco.
Chemically, alcohol is a depressant that acts on the central nervous system to alter mood, behavior, and mental state. Excessive amounts are considered highly toxic and dangerous because of its ability to:
These biological impacts can harm every part of our bodies in so many ways and increase the risks of developing chronic diseases like cancer.
It may be excruciatingly difficult to change your habits and quit drinking, especially if addiction has sunk its claws into every aspect of your life. Most alcoholics will quickly resume drinking to make the symptoms stop, which perpetuates the cycle of addiction.
It’s time to get the help you need. Contact Ardu Recovery Center. Our skilled professionals can help you every step of the way.
Learn more about our rehab and addiction treatment center.
Medical experts warn that the more you drink, the higher your chances of cancer.
Let’s look at the eight possible ways alcohol abuse and addiction to alcohol may lead to cancer:
Even if you drink at lower amounts and in controlled environments, alcohol has a greater potential to cause harm than good to your entire body. Read more about the effects drinking has on your brain.
We’re all guilty of enjoying an occasional unwinding with a drink without realizing alcohol’s insidious effects on cancer risk. But the research is clear: excessive drinking over time raises the likelihood of developing many malignancies.
A meta-analysis of 572 studies involving 486,538 cancer cases found that heavy alcohol consumption significantly increases the risk of:
The metabolism of alcohol inflicts serious damage to your whole body that paves the way to cancer development. Not only does its metabolism put an enormous amount of stress on your liver and other vital organs, but it also creates toxic byproducts along the way that wreak havoc at the cellular level.
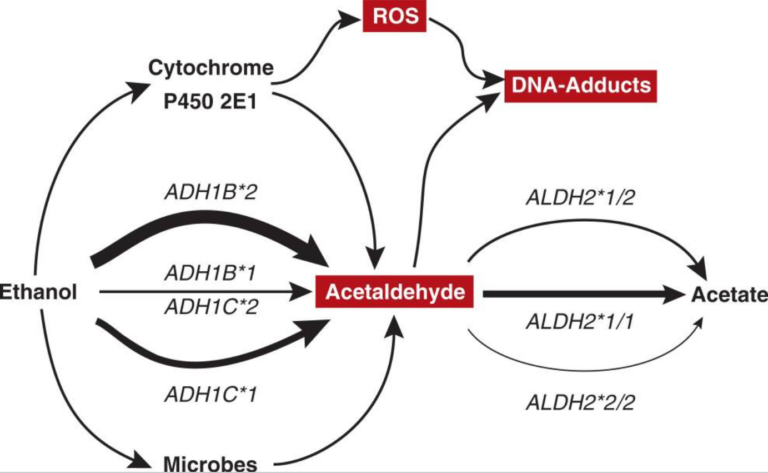
When you consume alcohol, your body breaks it down through multiple metabolic processes. The primary pathway involves two enzymes: alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH). In the liver, ADH initiates the breakdown by converting alcohol (ethanol) into acetaldehyde. Acetaldehyde is an intermediate metabolite and is highly toxic and carcinogenic.
…acetaldehyde induces inflammation and transformation of the cells lining the windpipe (i.e., trachea), interferes with the normal reproduction of cells, and enhances cell injury of the gastrointestinal mucosa associated with excessive cell growth. (Seitz et al)
Acetaldehyde is further metabolized by ALDH into a relatively harmless compound called acetate. This helps remove the harmful acetaldehyde from the body. Problems arise when acetaldehyde accumulates faster than ALDH can clear it. This large amount of acetaldehyde causes several issues:
Saying no to booze can be difficult, but our alcohol detox center can help you break the cycle of dependence and provide comprehensive treatment for alcohol addiction.
Oxidative stress is an imbalance between reactive oxygen species and antioxidants in the body. ROS are free radicals that damage cells through oxidation but antioxidants help neutralize them before they cause harm.
Alcohol disrupts the ROS-antioxidant balance in several ways:
The surplus of these free radicals creates oxidative stress. Oxidative stress, in turn, increases oxidation in the body, a process involved in mutation production. While our cells typically employ repair mechanisms to fix many of these mutations, some of them can allow cells to divide uncontrollably and form tumors.
The 2003 study also lists many factors that contribute to alcohol-induced oxidative stress:
Oxidative stress also triggers inflammation by activating cytokines and redox signaling pathways. One study investigated the association between alcohol consumption and oxidative stress and found that alcoholism can be seen as an inflammatory condition.
There is a clear-cut relation between oxidative damage and inflammation and alcoholism-associated diseases such as brain dysfunction, bone and muscle diseases, lung alterations, increased severity of infections, malnutrition, and an increased prevalence of cardiovascular disease or cancer. (González-Reimers, et. al.)
A 2002 study explains how excessive alcohol intake can harm the liver by releasing these cytokines. These substances trigger responses in liver cells, leading to cell death and damage. In response to this, the liver generates reactive oxygen and nitrogen species. The liver’s defense mechanisms become overwhelmed by alcohol’s damaging effects, leading to cancer death, which triggers even more inflammation.
It’s a vicious circle.
Your body goes through all kinds of vicious circles when it tries to process alcohol. Binge drinking really takes a toll on your body, and your internal organs are the first to take the fall. Frequent binge drinking can be symptomatic of larger alcohol addiction, so seek help as soon as possible.
Alcohol can compromise your body’s ability to properly absorb key nutrients from food and supplements. Several mechanisms bring harm to the gastrointestinal tract responsible for nutrient uptake.
Alcohol’s direct damage to the GI lining interferes with absorption. As an irritant, alcohol can inflame the mucosa of the mouth, esophagus, stomach, and intestines. This inflammation disrupts the function of enterocytes, the absorptive cells that line the GI tract. When enterocyte structure and metabolism are impaired, they cannot properly transport and process nutrients.
Research shows that chronic alcohol use can lead to malnutrition because of the way alcohol interferes with the absorption of important nutrients in the small intestine, such as glucose, vitamins B1, B2, B9, and C, as well as minerals like selenium, iron, and zinc.
…alcohol can impair the function of the muscles separating the esophagus from the stomach, thereby favoring the occurrence of heartburn. Alcohol-induced damage to the mucosal lining of the esophagus also increases the risk of esophageal cancer. (Bode and Bode)
Bode and Bode have also found that “alcohol may interfere with structure as well as the function of GI-tract segments.”
…alcohol inhibits the absorption of nutrients in the small intestine and increases the transport of toxins across the intestinal walls, effects that may contribute to the development of alcohol-related damage to the liver and other organs.
Alcohol can cause serious damage to the kidneys, liver, brain, and other vital parts of your body. Don’t wait too long before you turn to someone for help. Not only will you protect your mental health but also your physical health.
At Ardu, we help you heal both. Learn how our mental health treatments can help you on the path to recovery from alcohol addiction and overall well-being.
We can’t stress enough how terrible alcohol is for your liver. Even before we consider that it may increase the chances of getting liver cancer, alcohol addiction can lead to fatty liver, liver fibrosis, cirrhosis, and alcoholic hepatitis.
The bad news is all these forms of alcoholic liver disease may ultimately cause hepatic (liver) cancer. The good news is your liver possesses an incredible ability to heal if you stop drinking alcohol and start recovering. Here’s what happens to your liver when you call it quits with booze.
If you don’t quit drinking, alcoholic liver disease can set the stage for cancer.
Japanese researchers found more evidence that heavy and even moderate drinking can lead to cancer through several other mechanisms.
It is well known that alcohol interacts with other factors, such as cigarette smoking, viral hepatitis, and diabetes, leading to an increased risk of hepatocellular carcinoma. There are several possible mechanisms through which alcohol may induce liver carcinogenicity, including the mutagenic effects of acetaldehyde and the production of ROS due to the excessive hepatic deposition of iron.
The first few weeks after quitting may be the hardest on your liver, as alcohol withdrawal symptoms set in. We can help you and your liver in the process. We’re here to facilitate your recovery at our drug and alcohol rehab center.
Since we’re speaking about quitting, good things happen to your entire body when you do. Read about what happens to your brain when you say goodbye to booze.
Our hormones are like an intricate symphony: each player has a part in maintaining overall hormonal harmony. When you add alcohol to the equation, the symphony may turn into a bag of wailing cats. Even moderate drinking can profoundly impact hormone regulation, interfering with the balanced signaling that keeps cells functioning normally. This hormonal havoc that alcohol causes may be one reason behind alcohol’s links to higher cancer risk across organ systems.
Alcohol may promote cancer cell growth by disrupting hormonal homeostasis. This effect is best shown in breast cancer patients, in which excessive drinking may have elevated estrogen levels. that stimulates the growth and division of breast tissue cells. The more estrogen in your body, the higher the risk factor for developing breast cancer.
By increasing estrogen levels, alcohol creates an internal environment in breast tissue that enables malignant cells to develop and progress into breast tumors. Cancer research sheds light on how alcohol might aid tumor development through complex hormonal mechanisms.
IGF-1 protein levels were reduced in the hippocampus 48 h after binge-like alcohol exposure (oral gavage) in male and female rats, and 4 days of binge-like exposure reduced IGF-1 protein levels only in female rats. (Liran, et. al.)
…chronic alcohol exposure impairs folate absorption by inhibiting expression of the reduced folate carrier and decreasing the hepatic uptake and renal conservation of circulating folate. (Halsted, et. al.)
In case this wasn’t enough cancer-causing factors, alcohol also seems to deplete your melatonin levels.
Melatonin is the so-called “sleep” hormone involved in regulating circadian rhythms. It seems to pack some amazing anti-cancer properties. Melatonin can:
Too bad alcohol tends to drop your natural melatonin levels to the floor. A 2006 study found that the melatonin disruption seen in alcoholics may be due to long-term alcohol use. It might be linked to changes in the body’s internal timing system (circadian clock) during chronic alcohol consumption.
However, some researchers suggest that melatonin may have a protective effect against the harm caused by alcohol, particularly in the liver and the immune system.
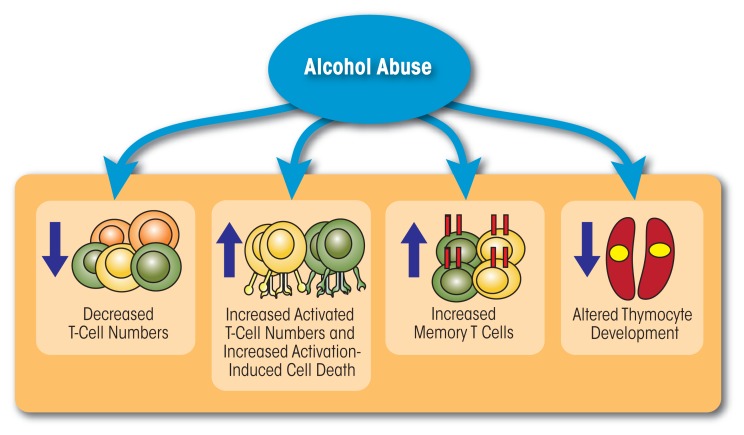
A robust immune system is a formidable barrier against cancer development and growth. But alcohol unleashes hell on immune cells and processes that maintain your health. Chronic drinking suppresses key immune surveillance mechanisms, helping malignancies to evade your immune system’s detection.
Alcohol impacts both the innate and adaptive branches of the immune system. Chronic exposure reduces circulating lymphocytes, hampering humoral and cell-mediated adaptive immunity. This includes impaired T-cell activation and proliferation in response to cancerous cells.
Let’s not even mention its pro-inflammatory effects that trigger oxidative stress, disturb the balance of cytokines, and create the perfect microenvironment that promotes tumor angiogenesis and growth rather than immune destruction.
Cancer research has discovered more ways in which alcohol weakens the immune function to promote cancer:
Alcohol causes dysbiosis of the gut microbiota in rodents and humans, as well as decreased production of beneficial metabolites such as short-chain fatty acids. (Zhang, et. al.)
The impact of alcohol on immune defenses is yet another reason to carefully consider your relationship with drinking. If you have a problem with binge drinking, there’s a high probability that you either struggle with alcohol addiction or are on your way to developing one.
The stages of alcoholism can sneak up on you before you even realize it. With compassion and tenacity, we can overcome addiction and equip our bodies to triumph against cancer. Learn how Ardu Recovery Center can help you stop binge drinking.
Losing oneself in the bottle may provide temporary comfort and relieve your stress, but this solace comes at a much greater cost. Alcohol is calorie-dense. It can pile on excess pounds, leading down the path of obesity and heightened cancer risk.
The hormonal, inflammatory, and metabolic changes that accompany obesity create the cellular conditions, growth-promoting signals, energy availability, and local tissue environment for cancers to thrive in.
Here’s what excessive amounts of alcohol do to your body:
A 2023 study reached some shocking conclusions. People who drank more than the recommended amounts of alcohol and were in the higher-weight categories had a greater risk of developing cancer. Similarly, higher levels of obesity were linked to more cancer risk, regardless of the levels of alcohol consumption.
…the joint association analyses showed that across all adiposity markers, above guideline drinkers who were in the top two adiposity groups had elevated cancer incidence risk…Regardless of alcohol consumption status, the risk of obesity-related cancer increased with higher adiposity in a dose–response manner within alcohol consumption categories.
Obesity and higher alcohol consumption levels together substantially raise colorectal cancer risk. Obese drinkers had 2.2 times higher risk than non-drinking obese people.
Among obese individuals, 3 or more different types of drinks were associated with a 3.4-fold higher risk of CRC relative to non-drinkers. The risk of CRC also increased with drinking years and drinks daily among obese participants. However, no increased risk was observed in people without obesity. (Zhao, et. al.)
Obesity and alcohol can synergize into a hazardous cocktail for cancer risk. We understand old habits die hard and progress rarely follows a straight path. That’s why our alcoholic detox program can help you get over the initial withdrawal stage, while our alcohol rehab teaches you how to rewire your patterns, body, and brain for an addiction-free life.
Another synergistic relationship with alcohol may be paving the road to cancer. Alcohol and tobacco are common vices that when combined, can significantly amplify your risk of developing certain cancers, especially of the mouth, throat, larynx, and esophagus.
According to the National Cancer Institute, on their own, smoking cigarettes and drinking can respectively spur 17 cancers or up to 7 cancers. Used side-by-side, they create a serious synergistic situation. If you light one cigarette while you’re consuming alcohol, the risk of developing cancers along the upper gastrointestinal tract (from mouth to lower esophagus) explodes.
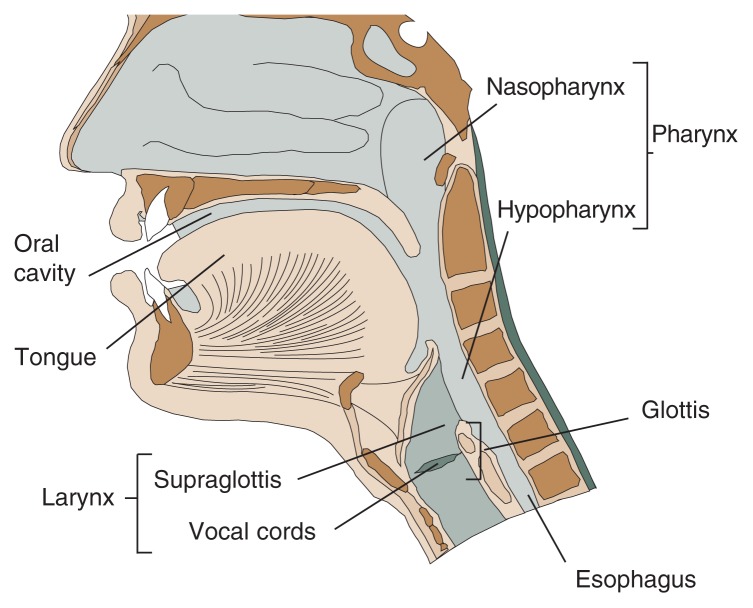
The parts of the mouth and throat that are more exposed to alcohol and tobacco are more susceptible to cancer. This also applies to voice box (larynx) cancer. Research shows that alcohol and tobacco together seem to increase the risk of esophageal squamous cell carcinoma synergistically: their combined impact is greater than the sum of their individual effects.
Several factors contribute to this dangerous synergistic effect:
There’s no going around it: the key steps to reducing carcinogenic risks from this dangerous cocktail of substances are to quit smoking and avoid alcohol.
At Ardu, we help you break the cycle of dependence on alcohol. Through our medically supervised detox, counseling, group support, and holistic rehab therapies, we help you break the cycle of alcohol addiction and reclaim lifelong wellness.
While genetic factors and bad luck play a role in cancer, researchers estimate nearly 40% of cancers can be prevented through lifestyle choices—one of the most important ones being cutting back on or completely ditching booze.
Here are some smart suggestions:
Recovery is a deeply personal journey. Rather than taking a one-size-fits-all approach, we at Ardu Recovery Center develop customized treatment plans tailored to your specific needs and goals.
Inpatient treatment at our residential facilities surrounds you with 24/7 support. Outpatient treatment programs, such as partial hospitalization and intensive outpatient programs, offer flexible solutions to maintain your home and work routines or receive treatment while in a sober living facility.
With psychotherapy and other modalities, you learn healthy coping skills so you aren’t tempted to rely on alcoholic beverages. A variety of therapeutic approaches, from cognitive behavioral therapy to motivational interviewing to dialectical behavioral therapy, allow you to find the modality that resonates with you.
If you have a co-occurring mental health disorder—such as anxiety, depression, or bipolar disorder—our dual diagnosis treatment program can help you heal both your alcohol addiction and your other mental health issues.
We do everything in our power to help you find your way back to wellness. Our comprehensive recovery program can aid you in restoring balance so cancer risks smolder no more.

Brandon Okey is the co-founder of Ardu Recovery Center and is dedicated to empowering people on their journey to sobriety.
Alcohol may affect people who were diagnosed with cancer differently. Alcohol is known to weaken the immune system, and cancer patients often have weakened immune responses due to their condition or cancer treatments like chemotherapy. This combination can make cancer patients more susceptible to infections and other complications.
Alcohol can also interact with some cancer medications, reducing their effectiveness and increasing side effects. It may also hinder the body’s ability to repair damaged tissues and can be particularly harmful if a patient is recovering from surgery.
On top of these concerns, alcohol is a source of empty calories, which can lead to weight gain, another risk factor for certain types of cancer. Alcohol may also interact with the body’s metabolic processes, potentially affecting treatment outcomes.
Discuss drinking alcohol with your healthcare providers to make sure you make the best, well-informed choices tailored to your specific situation.
Cancer is a complex disease with many different causes and risk factors. The primary factors contributing to cancer include genetics, environmental factors, lifestyle choices, and exposure to carcinogens.
While the exact causes can differ by cancer type, some common factors are well-established.
Alcohol is associated with an increased risk of several types of cancer. The International Agency for Research on Cancer (IARC) has classified alcohol as a Group 1 carcinogen, indicating that it is a known cause of cancer in humans.
Here are some of the cancers for which alcohol consumption is considered a risk factor:
The cancer risk associated with consuming a single drink is relatively low. While moderate alcohol consumption is generally considered safe and even associated with certain health benefits, even that one drink does carry some level of cancer risk. Alcohol, specifically ethanol, is classified as a Group 1 carcinogen by the International Agency for Research on Cancer (IARC). This means that there is sufficient evidence to confirm its role in the development of various cancers.
The risk is dose-dependent. The more alcohol you consume over time, the higher your risk of developing alcohol-related cancers. For instance, cancers of the oral cavity, throat, esophagus, and breast are linked to alcohol intake, and the risk increases with greater alcohol consumption.
The key lies in long-term, heavy, or binge drinking, which significantly raises the risk. If you’re concerned about cancer risk, reduce or eliminate alcohol consumption to make a sensible choice for your health.
Several individual factors determine a “safe” daily amount of alcohol consumption:
The U.S. Department of Health and Human Services and the U.S. Department of Agriculture define moderate drinking as up to one drink per day for women and up to two drinks per day for men. A standard drink is typically defined as containing about 14 grams (0.6 ounces) of pure alcohol.
These guidelines suggest that, for many adults, low-risk alcohol consumption is associated with limited or no cancer risk. However, take individual tolerance and susceptibility to alcohol into consideration. There are people who should avoid alcohol entirely, such as pregnant and breastfeeding women and people with certain medical conditions or a history of alcohol use disorder.
Taking a 40-day break from alcohol, often referred to as a “dry” period, can offer several potential benefits:
For those with a history of heavy or problematic drinking, a more extended period of abstinence or seeking professional help may be more helpful. Ultimately, a temporary break from alcohol can be a healthy choice.
While the relationship between sugar consumption and cancer is a topic of ongoing research, there is no conclusive evidence to support the direct causation of cancer by sugar. However, there are indirect links between sugar and cancer risk that are worth considering:
While the existing evidence does not definitively establish sugar as a direct cause of cancer, try to maintain a balanced diet and avoid excessive sugar intake as part of a cancer prevention strategy. A diet rich in fruits, vegetables, whole grains, and lean proteins is generally recommended for overall health and cancer risk reduction.
Liver cancer symptoms can vary depending on the stage and type of liver cancer, but they may include:
Liver cancer may not present symptoms in its early stages. As a result, it is often diagnosed at more advanced stages when symptoms become more noticeable. Routine screenings, especially for individuals at higher risk, can aid in early detection.
There is no type of alcohol that can be definitively considered as preventing cancer. While some studies have suggested that certain components of alcoholic beverages like red wine may have potential health benefits due to the presence of antioxidants like resveratrol, these findings are not conclusive, and their effectiveness in preventing cancer remains uncertain.
The risks associated with alcohol consumption, including its link to many cancer types, outweigh any potential benefits. Any positive effects of alcohol are generally not considered significant enough to promote its consumption for health reasons.
What is the best way to stop drinking?
Is alcoholic personality a myth?
What does alcohol do to the skin?
Why does drinking cause my skin to go red?
The economic cost of alcohol abuse
Is alcohol toxic for the brain?