Written by Brandon Okey. Mina Draskovic, B.Psy., reviewed this content for accuracy.
Regular alcohol consumption can increase the risk of mouth cancer.
A 2006 study published by Alcohol Research and Health found that approximately 80% of oral and pharyngeal cancer cases in men and about 65% of cases in women can be attributed to alcohol use.
Alcohol is extremely cancerous. Even moderate alcohol consumption is linked to an increased likelihood of developing several types of cancer. Research shows that worldwide, “an estimated 741 300, or 4.1%, of all new cases of cancer in 2020 were attributable to alcohol consumption”.
If you be free of an alcohol addiction, our rehab center can help. Contact Ardu Recovery Center and start the journey toward sobriety in a supportive and compassionate environment.
I recommend you go to ARDU if you or someone you know is struggling with addiction. You won’t find a better program!!! Thanks to my ARDU family, I now have 91 days in recovery today!
While moderate amounts of alcohol generally cause little harm to oral health, making a habit of regular or heavy drinking could lead to some painful issues down the road. Over time, too much alcohol helps nasty bacteria thrive while drying out protective saliva, paving the way for decay, gum disease, and infection.
Ethanol is the primary alcohol molecule found in alcoholic drinks. When processed by the liver, ethanol is converted to acetaldehyde, alcohol’s principal metabolite. Acetaldehyde has cytotoxic, dehydrating, and immunosuppressant properties that:
Indian researchers showed that “alcohol dependent subjects had slightly lower mean plaque and salivary pH and a higher prevalence of dental caries, periodontitis and mucosal lesions…” The study found a significantly higher prevalence of dental caries, periodontitis (89.61%), and mucosal lesions (31.5%) among alcohol-dependent subjects compared to nonalcoholics.
These effects, alongside a number of others, increase the risk of mouth, throat, and esophageal cancers.
Mouth cancer has overt symptoms, and excessive alcohol consumption makes them hard to ignore. The warning signs unique to oral cancers typically start to show after years of heavy drinking, so alcohol-related cases tend to be caught late.
Here are the symptoms of mouth cancer caused by alcohol:
If you notice any of these symptoms, contact your doctor right away to get examined. There are physical and psychological signs of alcohol addiction that can indicate the need to seek help before your health deteriorates.
If you believe your drinking has gotten out of hand and worry it may impact your health over time, contact Ardu and join our alcohol addiction treatment program. Don’t ignore the red flags.
A meta-analysis of 572 studies involving 486,538 cancer cases found that heavy alcohol consumption significantly increases the risk of many types of cancer including liver carcinoma, breast cancer, pancreatic cancer, laryngeal cancer, esophageal cancer, and oral cavity cancer.
There are several ways alcohol consumption can cause mouth cancer.
Alcohol metabolism creates a toxic environment that allows cancer to thrive. When the body breaks down alcohol, it produces acetaldehyde, a toxic chemical that damages DNA and prevents cells from repairing properly.
Scientific research has shown that acetaldehyde is a known carcinogen. It can bind to DNA and interfere with DNA replication, causing mutations that lead to cancerous growths. The American Cancer Society highlights that alcohol can act as an irritant, especially in the mouth and throat, leading to DNA changes that may lead to cancer.
Some of the acetaldehyde produced during alcohol metabolism makes its way into saliva. Prolonged exposure to acetaldehyde in saliva can promote tumor growth along the digestive tract, from the mouth to the esophagus and stomach.
Acetaldehyde is found in the saliva, which can lead to an elevated risk of oropharyngeal cancer. Cancer risk increases with the amount of acetaldehyde generated in the saliva, and patients with oropharyngeal cancer have elevated acetaldehyde concentrations in their saliva. (Seitz and Becker)
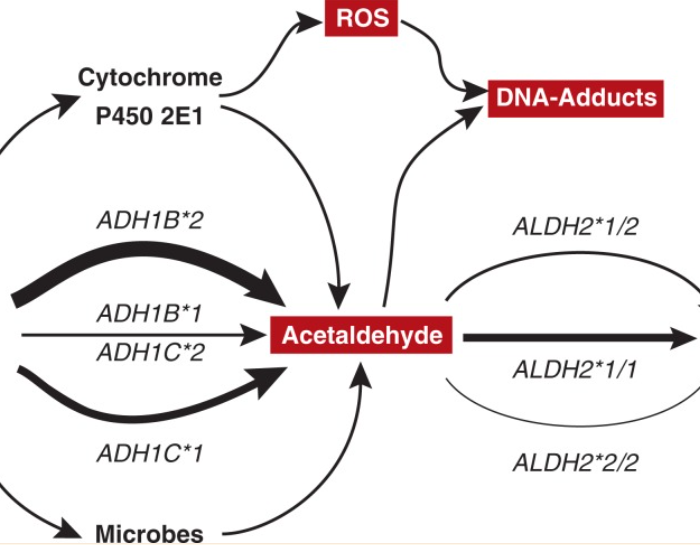
As alcohol metabolism generates toxic acetaldehyde, this chemical literally binds to DNA and alters its structure. Your body tries hard to repair DNA damage, but heavy drinking overwhelms these repair systems.
Persistent DNA damage from alcohol metabolism can lead cells to make copying mistakes during replication. The result is a possible mutation that triggers uncontrolled cell growth. French researchers found that many types of cancer—including cancers of the upper aerodigestive tract—are caused by the way alcohol damages DNA.
Ethanol’s metabolite acetaldehyde can cause DNA damage and block DNA synthesis and repair, whilst both ethanol and acetaldehyde can disrupt DNA methylation. Ethanol can also induce inflammation and oxidative stress leading to lipid peroxidation and further DNA damage.
This is why long-term heavy drinkers often develop those ominous red or white mouth patches that can be precursors for mouth cancer.
Heavy drinking can mess with your gut’s ability to soak up nutrients from food. Alcohol is an irritant that inflames the delicate lining of your digestive tract from the mouth to the intestines. When these tissues get angry and swollen, the cells responsible for shuttling nutrients from food can’t do their job, leaving your body deficient and susceptible to damage that sparks cancer.
…alcohol can impair the function of the muscles separating the esophagus from the stomach, thereby favoring the occurrence of heartburn. Alcohol-induced damage to the mucosal lining of the esophagus also increases the risk of esophageal cancer. (Bode and Bode)
At Ardu, we know how important nutrition is during recovery. Our nutritional therapy program helps you on your path to sobriety and well-being. Our nutritionists work closely with you to develop eating plans, and advice on supplements, and offer nutrition education, all part of supporting the body’s natural ability to heal and recover.
Did you know that alcohol triggers widespread inflammation in your body? Each sip of that stiff cocktail or bitter beer puts your mouth in direct contact with ethanol, which irritates and inflames your oral cavity.
Some studies have indicated that cirrhosis of the liver due to alcohol intake may be associated with an increased risk for oral cancer. A 2018 study published by the British Dental Journal found that alcohol causes “damage to the liver which is then less able to deal with potentially carcinogenic substances.”
While an occasional drink may only cause slight redness of the oral cavity, years of exposure can really add up. Persistent inflammation drives mouth cells to divide more often to replace damaged tissue. And every time cells divide, there are more chances for DNA copying mistakes that yield permanent mutations. So, more alcohol consumption can provoke precancerous changes.
Alcohol devastates immune system functioning, enabling cancers to sneak past detection. Both innate and adaptive immunity are hit, with fewer lymphocytes in circulation. T-cell responses weaken, leaving the body unable to stop tumor development.
T-cells or T-lymphocytes are natural cancer cell killers that may even stimulate and recruit other immune cells to crank up their anti-tumor response. Cancer research has discovered alcohol reduces T-cells that detect and kill cancerous cells.
Toxic byproducts also spark bodily inflammation, disturbing immune balance and allowing tumors to proliferate rather than die off.
The impact of alcohol on immune defenses is another reason to carefully consider your relationship with drinking. If you can’t stop binge drinking, there’s a high probability that you either struggle with an alcohol addiction or are on your way to developing one.
Our alcohol detox program can help you get through the initial withdrawal stage safely, teaching you how to rewire your patterns, body, and brain for an addiction-free life.
The statistics on alcohol and oral cancer indicate a clear association between alcohol consumption and the risk of developing oral cancer. Rumgay, et. al. found that “approximately 4% of cancers worldwide are caused by alcohol consumption.”
The British Dental Journal states that the risk of mouth cancer increases with greater alcohol intake, with a 20% increased risk associated with low alcohol intake. This means that even a small or moderate intake of alcohol appears to be linked to higher chances of developing mouth cancer versus not drinking at all.
Some studies focus on the joint exposure of alcohol and tobacco on oral health and the development of mouth cancer, revealing that they increase each other’s harmful effects. The National Cancer Institute reveals that alcohol may make the mouth more absorbent, allowing tobacco carcinogens to enter the body more easily.
Chinese researchers have confirmed the detriment of combined exposure to alcohol and tobacco smoke and revealed that “both smoking and drinking are involved in mouth neoplasms, oral cancer, leukoplakia, and periodontal diseases.”
To curb cancer risk, choose health—let go of drinking and smoking. Through our medically supervised detox, counseling, group support, and holistic rehab therapies, we help you break the cycle of alcohol addiction and reclaim lifelong wellness.
Based on what we’ve discovered so far, the cancer risk from alcohol consumption is far from overstated. On the contrary, alcohol has been conclusively linked to cancers of the mouth, throat, esophagus, liver, colon, rectum, and breast.
In a 2020 study, patients who developed oral cavity cancers tended to be current drinkers who consumed alcohol at higher intensities compared to cancer-free individuals. For those with cancers of the throat (oropharynx, hypopharynx) or larynx, very few were non-drinkers, indicating that drinking alcohol was a strong risk factor. Those patients also drank more heavily over longer periods, further implicating alcohol’s role in many head and neck cancer cases.
The research clearly demonstrates a dose-dependent relationship: the more alcoholic beverages you have, the higher your cancer risk, especially with consistent consumption.
Read more about how much alcohol is detrimental to your health.
There is evidence that suggests that when you reduce alcohol consumption, you may face a lower risk of alcohol-related cancers, including cancer of the mouth. A Korean cohort study found that increasing alcohol consumption raises cancer risk while abstinence and intake reduction lowers cancer risk.
A 2008 study published in Pharmaceutical Research showed that alcohol consumption had been linked to 15-20% of cancer deaths, prompting recommendations to moderate intake. They concluded that cessation or reduction in the amount of alcohol you consume is considered a necessary lifestyle change to help prevent up to a third of common cancers, including mouth cancer.
It may be difficult to change your habits and lifestyle and quit drinking. Most alcoholics will quickly relapse to curb the withdrawal symptoms, which only perpetuates the cycle of addiction.
Contact Ardu Recovery Center and get the support you need.
Anyone struggling with alcohol abuse or addiction is welcome in our alcohol addiction treatment program. We help people overcome their addictions and restore all aspects of their well-being. Rather than taking a one-size-fits-all approach, we at Ardu Recovery Center develop customized treatment plans tailored to your specific needs and goals.
Inpatient treatment at our residential facilities surrounds you with 24/7 support. Outpatient treatment programs, such as partial hospitalization and intensive outpatient programs, offer flexible solutions to maintain your home and work routines or receive treatment while in a sober living facility.
With psychotherapy and other modalities, you learn healthy coping skills so you aren’t tempted to rely on alcoholic beverages for comfort or relief. Our therapeutic approaches—from cognitive behavioral therapy and motivational interviewing to dialectical behavioral therapy—allow you to find the modality that resonates with you.
Getting proper treatment empowers you to manage alcoholism while implementing lifestyle changes that will help you heal. With compassion and expertise, we can help you achieve lasting sobriety and get your health back on track.

Brandon Okey is the co-founder of Ardu Recovery Center and is dedicated to empowering people on their journey to sobriety.
A 2014 meta-analysis found that heavy alcohol consumption is a significant risk factor for:
Frequent alcohol consumption is an independent risk factor for developing periodontal diseases like gingivitis and its more severe form, periodontitis. This direct association arises because alcohol creates an imbalance in oral bacteria, allows more growth of plaque, and causes inflammation in gum tissues and bone supporting the teeth. Heavy drinkers tend to neglect proper oral hygiene as well. All of these alcohol-related factors contribute to progressive gum disease.
Studies confirm that heavy, long-term alcohol use does lead to gum recession by drying out the oral mucosa and reducing saliva production, making tissues vulnerable to shrinkage. Tezal, et. al. assessed the relationship between alcohol consumption and the severity of periodontal disease, and concluded that alcohol consumption is associated with higher gingival bleeding and more severe clinical attachment loss.
Alcohol’s irritating nature also elicits inflammatory chemicals that can damage the gums and supporting bone tissue, allowing them to detach and recede from the teeth. Those who drink excessively over many years often exhibit receding, shrinking gums as oral issues accumulate.
Chronic excessive alcohol consumption can affect the tongue in several ways. Deficiencies in B vitamins like folate due to heavy drinking commonly cause a swollen, reddened, sore tongue known as glossitis. Alcoholics may also develop glossodynia, which is characterized by a painful, burning tongue. Direct contact with alcohol causes irritation and changes in tongue papillae, while toxins from liver disease lead to a distinctive musty, bad breath. Poor immunity makes drinkers more prone to fungal infections and cancerous lesions on the tongue over time.
Dentists can recognize both physical and behavioral signs of heavy drinking. Oral indicators include dental erosion, gum disease, tissue irritation, halitosis, oral cancer, etc. Psychological signs like avoiding hygiene discussions, canceling appointments, anxiety, and depression may also indicate alcohol abuse problems. Skilled dentists consider these observations during checkups to determine if a patient’s oral health is being impacted by excessive alcohol intake.
The prognosis for oral cancer varies by stage, with 5-year survival over 80% when detected early. The survival rate decreases to 65% and 38% once the cancer spreads. Prognosis depends on location, how advanced the disease is when diagnosed, and response to surgery, radiation, chemotherapy, etc. Early recognition of symptoms and medical intervention improves prognosis.
Oral cancer is extremely painful because growing tumors infiltrate the dense network of sensitive nerves supplying the mouth and throat areas. Tumors damage surrounding tissue, bone, and muscle, releasing compounds that severely irritate nerve fibers. Pain worsens as lesions erode further. Oral cancer treatments such as surgery, chemotherapy, and radiation also contribute to nerve pain.
Pelucchi, C., Gallus, S., Garavello, W., Bosetti, C., & Vecchia, C. L. (2006). Cancer Risk Associated with Alcohol and Tobacco Use: Focus on Upper Aero-digestive Tract and Liver. Alcohol Research & Health, 29(3), 193-198. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6527045/
Rumgay H, Shield K, Charvat H, Ferrari P, Sornpaisarn B, Obot I, Islami F, Lemmens VEPP, Rehm J, Soerjomataram I. Global burden of cancer in 2020 attributable to alcohol consumption: a population-based study. Lancet Oncol. 2021 Aug;22(8):1071-1080. doi: 10.1016/S1470-2045(21)00279-5. PMID: 34270924; PMCID: PMC8324483.
Priyanka, K., Sudhir, K. M., Sekhara Reddy, V. C., Kumar, R. K., & Srinivasulu, G. (2017). Impact of Alcohol Dependency on Oral Health – A Cross-sectional Comparative Study. Journal of Clinical and Diagnostic Research : JCDR, 11(6), ZC43. https://doi.org/10.7860/JCDR/2017/26380.10058
Bagnardi, V., Rota, M., Botteri, E., Tramacere, I., Islami, F., Fedirko, V., Scotti, L., Jenab, M., Turati, F., Pasquali, E., Pelucchi, C., Galeone, C., Bellocco, R., Negri, E., Corrao, G., Boffetta, P., & Vecchia, C. L. (2015). Alcohol consumption and site-specific cancer risk: A comprehensive dose–response meta-analysis. British Journal of Cancer, 112(3), 580-593. https://doi.org/10.1038/bjc.2014.579
How does alcohol cause cancer? (2023, September 6). Cancer Research UK. https://www.cancerresearchuk.org/about-cancer/causes-of-cancer/alcohol-and-cancer/how-does-alcohol-cause-cancer
Alcohol Use and Cancer. (n.d.). American Cancer Society. https://www.cancer.org/cancer/risk-prevention/diet-physical-activity/alcohol-use-and-cancer.html
Seitz, H. K., & Becker, P. (2007). Alcohol Metabolism and Cancer Risk. Alcohol Research & Health, 30(1), 38-47. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3860434/
Rumgay, H., Murphy, N., Ferrari, P., & Soerjomataram, I. (2021). Alcohol and Cancer: Epidemiology and Biological Mechanisms. Nutrients, 13(9). https://doi.org/10.3390/nu13093173
Bode, C., & Bode, J. C. (1997). Alcohol’s Role in Gastrointestinal Tract Disorders. Alcohol Health and Research World, 21(1), 76-83. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6826790/
Ogden, G. R. (2018). Alcohol and mouth cancer. British Dental Journal, 225(9), 880-883. https://doi.org/10.1038/sj.bdj.2018.921
Pasala, S., Barr, T., & Messaoudi, I. (2015). Impact of Alcohol Abuse on the Adaptive Immune System. Alcohol Research : Current Reviews, 37(2), 185-197. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4590616/
Liu, H., Yu, Z., Xu, Z., Liu, T., & Liu, W. (2023). A scientometric study of tobacco and alcohol use as risk factors for oral cavity health. Journal of Dental Sciences, 18(4), 1883-1888. https://doi.org/10.1016/j.jds.2023.05.016
Di Credico, G., Polesel, J., Dal Maso, L., Pauli, F., Torelli, N., Luce, D., Radoï, L., Matsuo, K., Serraino, D., Brennan, P., Holcatova, I., Ahrens, W., Lagiou, P., Canova, C., Richiardi, L., Healy, C. M., Kjaerheim, K., Conway, D. I., Macfarlane, G. J., . . . Edefonti, V. (2020). Alcohol drinking and head and neck cancer risk: The joint effect of intensity and duration. British Journal of Cancer, 123(9), 1456-1463. https://doi.org/10.1038/s41416-020-01031-z
Yoo, J. E., Han, K., Shin, D. W., Kim, D., Chun, S., Jeon, K. H., Jung, W., Park, J., Park, J. H., Choi, K. S., & Kim, J. S. (2022). Association Between Changes in Alcohol Consumption and Cancer Risk. JAMA Network Open, 5(8). https://doi.org/10.1001/jamanetworkopen.2022.28544
Anand, P., Kunnumakara, A. B., Sundaram, C., Harikumar, K. B., Tharakan, S. T., Lai, O. S., Sung, B., & Aggarwal, B. B. (2008). Cancer is a Preventable Disease that Requires Major Lifestyle Changes. Pharmaceutical Research, 25(9), 2097-2116. https://doi.org/10.1007/s11095-008-9661-9
Tezal M, Grossi SG, Ho AW, Genco RJ. The effect of alcohol consumption on periodontal disease. J Periodontol. 2001 Feb;72(2):183-9. doi: 10.1902/jop.2001.72.2.183. PMID: 11288791.
If consumption of alcohol stops, does the liver heal?
Are my drinking habits genetic?
What is the role of alcohol on pancreatitis?
Is alcohol a major risk factor for obesity?
Can heavy exposure to alcohol lead to gout?
Is chronic alcohol intake bad for the heart?
Is beer consumption the culprit for the beer belly?