Written by Brandon Okey. Mina Draskovic, B.Psy., reviewed this content for accuracy.
Ever wonder what a night of drinking does to your pancreas? Excessive drinking has been directly linked to inflammation of the pancreas, which is more commonly known as pancreatitis.
Klockhov, et. al. revealed that “recurrent bouts of acute pancreatitis are associated with progression to chronic pancreatitis and are more common in chronic abusers of alcohol.”
Alcohol-induced inflammation damages pancreatic cells and disrupts the normal functioning of enzymes, leading to this painful and potentially serious condition.
This chronic inflammation sparked by one too many drinks can wreck your health. If you or someone you know is struggling with alcohol addiction, help is available.
Our rehab center in Provo, Utah can help you break the cycle of alcohol addiction through comprehensive treatment programs. These include medically monitored alcohol detox, psychotherapy, group support, and aftercare planning.
The pancreas is a long, flat organ that is vital to the digestive and endocrine systems. It is both an organ as well as a gland.
Proper functioning of the pancreas is paramount for overall well-being. It plays the following vital roles:
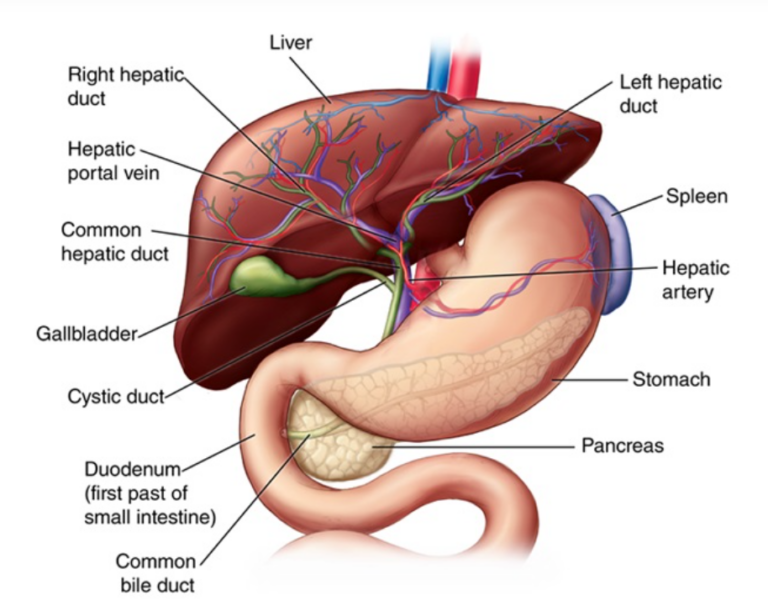
The pancreas collaborates with the liver in the breakdown and absorption of nutrients. Together, they ensure effective digestion, nutrient utilization, and maintenance of metabolic balance in the body.
Here’s how these two powerhouse organs team up:
These two organs are incredibly important for your health, so treat them with care. Many people suffer from impaired liver or pancreas function, especially those who indulge in regular binge drinking or develop alcohol dependency over years of heavy drinking.
Alcohol can wreak havoc on your liver, and it doesn’t treat your pancreas any better.
The pancreas is extremely susceptible to the toxic effects of alcohol. While low to moderate alcohol consumption may not immediately raise alarms, chronic alcohol abuse can cause a myriad of detrimental effects on your pancreas.
Here are some of the most notable effects:
Your liver thrives when you ditch alcohol, and the same is true with the pancreas. When you take alcohol out of the equation, your pancreas can gradually heal, reduce inflammation, restore enzyme production, and reclaim its pivotal role in digestion.
What are you waiting for? Contact Ardu and start your journey to recovery today.
Pancreatitis is an inflammatory condition of the pancreas. This potentially life-threatening and often chronic disease disrupts the delicate functions of the pancreas, leading to a wide range of complications, and in some severe cases, death.
Here’s how pancreatitis unfolds:
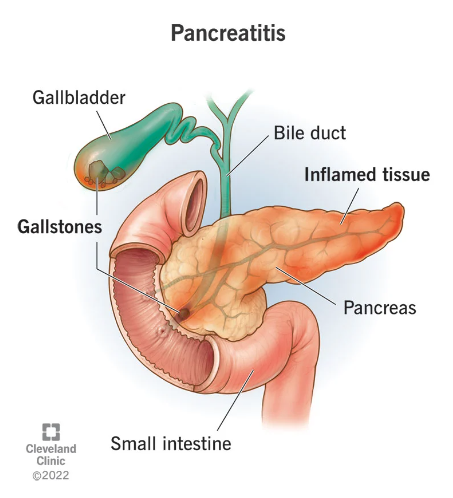
Inflammation can be triggered by many different factors.
While acute pancreatitis refers to a single instance of inflammation, excessive alcohol use often leads to persistent inflammation of the pancreas. Alcohol-induced pancreatitis is one of the most common conditions of which alcohol is the primary trigger.
Heavy, regular drinking impairs normal pancreatic function in many ways. With that being said, chronic inflammation is the true culprit of pancreatitis.
The pancreas will try to compensate for the damaging impact at first, but the more you drink, the more exhausted your pancreas becomes. Soon, it is unable to function properly.
Here’s what happens when you flood your pancreas with booze:
Repeated bouts of acute inflammation from direct ethanol effects slowly damage the pancreas beyond repair. Some experts say that mild or occasional drinking poses little risk, while heavy consumption burns out the organ.
We say it’s time to ditch the bottle. It isn’t always easy to quit, especially if addiction has sunk its claws into every aspect of your life. Many alcoholics will relapse and resume drinking, often in an attempt to curb withdrawal symptoms. Sadly, this only serves to perpetuate the cycle of addiction.
Contact Ardu Recovery Center to get the alcohol counseling and treatment you need.
Symptoms of alcohol-induced pancreatitis manifest similarly to other forms of pancreatitis. Like other types, alcohol-induced inflammation of the pancreas is extremely painful.
Here are the symptoms of alcoholic pancreatitis:
Pain from inflammation is a cardinal symptom in all forms of pancreatitis. In alcoholic pancreatitis, abdominal tenderness, and distention alongside nausea and increased heart rate are telling signs of the toxicity of alcohol.
Did you know that alcohol is also toxic to your brain?
Apte et al found that “the risk of developing pancreatitis increases with increasing doses of alcohol, suggesting that alcohol exerts dose-related toxic effects on the pancreas.” Klockhov, et. al. revealed that acute pancreatitis “usually manifests in patients with over five years of ongoing, substantial alcohol use (~4-5 drinks daily) and only rarely occurs from isolated binge drinking.”
Vonlaufen, et. al., however, offer a different take, explaining that “less than 10 percent of heavy alcohol users (180 g/day or about 15 drinks per day for 10 to 15 years) eventually develop clinically overt alcoholic pancreatitis.”
Here’s what you need to know about the relationship between alcohol and pancreatitis:
If you have a problem with binge drinking or find yourself unable to quit, there’s a high probability that you are either struggling with addiction or are at risk for developing a problem. Read our guide to the tell-tale physical symptoms of alcohol addiction.
Alcohol withdrawal can exacerbate inflammation in acute pancreatitis.
Here are some of the reasons why:
It’s important to manage withdrawal early on, especially in hospitalized alcoholic pancreatitis patients. The quicker you intervene, the lower the risk of life-threatening delirium tremens or alcohol withdrawal syndrome.
Our medical detox program can help you get through the initial stages of withdrawal, while our alcohol rehab program teaches you how to rewire your patterns, body, and brain to live an addiction-free life.
Alcoholic pancreatitis can severely shorten a person’s lifespan. Research shows that around half of patients with alcohol-related pancreatitis die within 20 years of disease onset.
Only 20 percent of deaths occurring before a patient’s life expectancy are attributed to pancreatitis or its complications; most of these deaths are attributed to the toxic effects of alcohol or smoking on other organs such as the liver. (Apte, et. al.)
A 2023 study revealed that patients with chronic alcoholic pancreatitis have a 95.5% one-year survival rate after surgery. Long-term prognosis tends to decline significantly with 63.5% of patients living 10 years post-operation.
This complex condition requires a comprehensive treatment plan that tackles substance use, chronic pain, nutrition, and other factors.
There are several key aspects to treating alcoholic pancreatitis:
Some people with acute pancreatitis have an alcohol dependency and need support to stop drinking. If this is you, contact Ardu today and start your recovery journey.
Recovery is a personal journey. Rather than taking a one-size-fits-all approach, the Ardu team develops customized treatment plans tailored to your specific needs and goals.
Inpatient treatment at our residential facilities surrounds you with 24/7 support. Outpatient treatment programs, such as partial hospitalization and intensive outpatient programs, offer flexible solutions to maintain your home and work routines or receive treatment while in a sober living facility.
With psychotherapy and other modalities, you learn healthy coping skills so you aren’t tempted to rely on alcoholic beverages. A variety of therapeutic approaches—from cognitive behavioral therapy and motivational interviewing to dialectical behavioral therapy—allow you to find the modality that resonates with you.
If you have a co-occurring mental health disorder, our dual diagnosis treatment program and mental health treatment plan can help you deal with alcohol addiction as well as other mental health issues.
Alcoholism and mental health issues often go hand in hand, and we do everything in our power to help you find your way back to wellness. Our comprehensive recovery program can aid you in restoring a healthy, well-balanced lifestyle.

Brandon Okey is the co-founder of Ardu Recovery Center and is dedicated to empowering people on their journey to sobriety.
Alcoholic pancreatitis can lead to death, both directly from disease progression and indirectly through systemic complications. As previous studies have shown, 50% of patients die within 20 years of diagnosis, and over a third sooner than the general population. Just 20% of these premature deaths directly result from chronic pancreatic injury.
The immune, endocrine, and digestive dysfunction induced by alcoholic pancreatitis can leave chronic pancreatitis patients severely debilitated and vulnerable to a cascading decline in health. Acute flare-ups of alcohol-related inflammation can result in organ failure, uncontrolled bleeding, infection, and other life-threatening issues. Over time, chronic pancreatic damage also raises the risk of diabetes, malnutrition, cancer of the gastrointestinal tract, and liver disease.
An acute pancreatitis episode can start just 48 hours after a binge drinking session. It often requires five or more years of continued alcohol intake for chronic alcohol-induced pancreatic injury from recurrent attacks to accumulate. Both acute and chronic alcohol-induced pancreatitis leave patients vulnerable to frequent acute flare-ups. The accumulation of inflammation that alcohol triggers can quickly spark swelling, pain, and systemic complications due to the destruction of pancreatic tissue over time.
The metabolism of ethanol generates significant oxidant stress which inflames tissues through its toxic byproducts. Alcohol causes protein deficiency, impairs protein response, and causes fatty liver, fibrosis, and cirrhosis, compromising cell integrity in both the liver and pancreas. Chronic ethanol administration can lead to alcoholic liver disease over time.
Specialized pancreatic stellate cells activate and release collagen scar tissue when chronically stimulated. Both vital organs suffer substantial structural and functional damage from the effects of alcohol consumption.
There is a wide range of characteristic symptoms that indicate pancreatic damage from alcohol. These include:
Blood labs measure elevated pancreatic enzymes and tests like CT scans reveal ductal calcifications and parenchymal scarring that is indicative of alcohol damage.
If chronic pancreatitis patients display these symptoms and indicators, it may mean that pancreatic tissue damage from alcohol has occurred.
The pancreas has remarkable regenerative capabilities. When given enough time and care, it can undergo a healing process, particularly when mitigating factors such as alcohol use disorder (AUD). Its repair also depends on the severity of alcohol dependence, the type of alcohol consumed, and the extent of long-term alcohol consumption.
Things like hereditary factors, environmental factors, and lifestyle choices can hinder the pancreas’ healing process.
It’s important to adopt a healthy lifestyle that will combat the development of pancreatitis. Make sure you incorporate clinical recommendations from your doctor and support your pancreas’ natural repairing process.
When you put an end to chronic alcohol consumption, you give your pancreas a chance to heal. This means acute or chronic cases of pancreatitis may potentially be resolved.
It’s important to address the detrimental effects of alcohol metabolites—such as acetaldehyde and reactive oxygen species. Address biological and environmental factors so your pancreas can recover from recurrent attacks.
Post-pancreatitis drinking (regardless of the amounts of alcohol) may trigger significant harm thanks to vulnerability caused by previous inflammatory damage. There is a substantial risk of experiencing recurrent episodes of pancreatitis even after years of abstinence.
If you suffered from alcoholic pancreatitis in the past, even an occasional drink might trigger some of the following:
People with a history of diagnosed pancreatic inflammation should abstain from the consumption of alcohol. To preserve precious pancreatic integrity, enzyme output, glycemic control, nutritional status, and overall health and prevent acute attacks of pancreatitis, work towards lifelong sobriety and vitality.
According to research, less than 5% of chronic, heavy drinkers get diagnosed with clinical pancreatitis.
In a population of 10%-15% of heavy drinkers, 2%-5% of all PC cases could be attributed to alcohol consumption. However, as only a minority (less than 10% for pancreatitis and 5% for PC) of heavily drinkers develops these pancreatic diseases, there are other predisposing factors besides alcohol involved. (Herreros-Villanueva, et. al.)
Researchers have analyzed predisposing factors such as alcohol metabolism, smoking, dietary co-factors (e.g., high-fat content, presence of infections), and calcium levels that may promote pancreatic cell injury. With that being said, no firm causative links have been found to explain why most drinkers avoid developing pancreatitis despite their alcohol-drinking habits.
To protect your pancreas, it’s best to limit drinking—or better yet, cut out alcohol altogether. The effects of ethanol on the human pancreas are toxic and destructive, so even acute episodes of binge drinking may inflict damage.
It’s important to maintain a balanced, low-fat diet, stay properly hydrated, and promptly treat any infections or conditions that could act as a trigger factor. It’s always best to seek medical care if you’re concerned about potential pancreatic symptoms.
While the human body can bounce back from acute attacks if they are spaced apart, consistent chronic damage can lead to loss of function.
Klochkov, A. (2023, May 16). Alcoholic Pancreatitis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK537191/
Mizumoto, A., Ohashi, S., Hirohashi, K., Amanuma, Y., Matsuda, T., & Muto, M. (2017, September 10). Molecular Mechanisms of Alcohol to Acetaldehyde-Mediated Carcinogenesis in Squamous Epithelium. International Journal of Molecular Sciences. https://doi.org/10.3390/ijms18091943
Vonlaufen, A. (2007). Role of Alcohol Metabolism in Chronic Pancreatitis. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3860433/
Apte MV, Pirola, R. C., & Wilson J. S. (2010, November 23). Mechanisms of alcoholic pancreatitis. Journal of Gastroenterology and Hepatology. https://doi.org/10.1111/j.1440-1746.2010.06445.x
Samokhvalov, A. V., Rehm, J., & Roerecke, M. (2015, December 1). Alcohol Consumption as an Additional Risk Factor for Acute and Chronic Pancreatitis: A Systematic Review and a Series of Meta-analyses. EBioMedicine. https://doi.org/10.1016/j.ebiom.2015.11.023
Wilson, G. C., Turner, K. M., Delman, A. M., Wahab, S. A., Ofosu, A., Smith, M. T., Choe, K. A., Patel, S. H., & Ahmad, S. A. (2023, March 15). Long-Term Survival Outcomes after Operative Management of Chronic Pancreatitis: Two Decades of Experience. Journal of the American College of Surgeons. https://doi.org/10.1097/xcs.0000000000000575
Herreros-Villanueva, M., Hijona, E., Bañales, J. M., Cosme, A., & Bujanda, L. (2013). Alcohol consumption on pancreatic diseases. World Journal of Gastroenterology: WJG, 19(5), 638-647. https://doi.org/10.3748/wjg.v19.i5.638
How much alcohol is too much to drink?
How do I know if I have an alcoholic personality?
What are the health risks of alcohol for men?
Can alcohol mess with birth control?
How does heavy drinking impact the brain?
Is beer the cause of the “beer belly”?
What is a high-functioning alcoholic?